Think Kids is a child psychologist practice which specialises in implementing customised therapy plans for children with special needs aged from 18 months to early adulthood.
Our highly experienced team of child psychologists and behaviour therapists take a holistic, evidence-based approach to help special needs children improve their quality of life. Our therapy involves collaboration with parents, caregivers and educators to achieve the best outcomes for your child.
Click here to see the Think Services flyer.
Led by our team of child psychologists, we take a disciplined approach to intervention and only implement proven, evidence based methods of therapy to bring out the best in your child.
Applied Behaviour Analysis (ABA) is the gold standard therapy for Autism, ADHD & behavioural challenges in children.
We use evidence-based methods to teach your child how to engage, regulate and respond to social interactions.
We provide a full range of diagnostic and psychometric assessments for children that are recognised by MoE and internationally.
Think Kids has a team of more than 20 child psychologists, behaviour therapists and ABA therapists who specialise in supporting children with special needs.
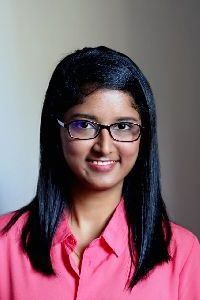
Below are profiles of some of our child psychologists. To view our full team please click here.



Our 10+ year track record and experienced child psychologist and ABA therapist team speaks for itself. Give your child their best chance in life.
Proven track record of more than 10 years
Customised therapy by child psychologists and ABA therapists
Home & centre based therapy options
Assessments recognised by MoE & schools
Open Monday to Saturday
Our team are accredited and registered with many professional psychological bodies to ensure the highest quality therapy for your child.















Our track record speaks for itself.
To schedule a no obligations appointment with one of our child psychologists, please either call us on +65 6735 4438 or Whatsapp +65 9853 6741 or email info@think-kids.com or fill out the enquiry form below.